Diabetic Eye Disease
As diabetes has become more common in the United States, so have eye conditions associated with diabetes. The most serious of these conditions, diabetic retinopathy, affects more than 4.4 million people. Diabetic retinopathy is considered to be the leading cause of new cases of blindness among adults, ages 20 to 74 years old. Diabetes can also lead to the development of cataracts and glaucoma.
OCB offers comprehensive care for diabetic retinopathy and other diabetes related eye disorders with the full range of advances in medication, laser and surgical options. Early detection, early intervention and ongoing monitoring as recommended by your OCB eye doctor are the best defense against diabetes related eye problems.
What is Diabetic Retinopathy?
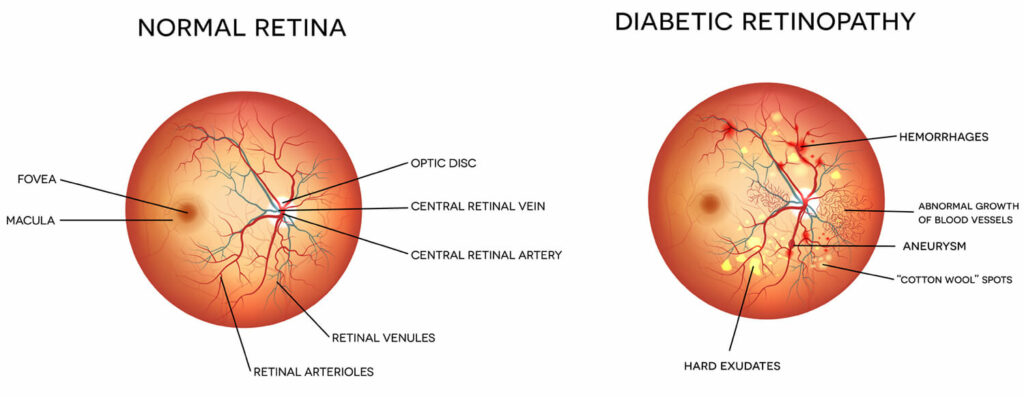
Diabetic retinopathy, the most common diabetic eye disease, occurs when abnormal blood sugar levels, brought on by diabetes, damage the blood vessels of the retina. Sometimes these vessels swell and leak fluid or even close off completely. In other cases, abnormal new blood vessels grow on the surface of the retina. If left untreated, this damage can lead to permanent vision loss and eventually blindness.
Unfortunately, diabetic retinopathy has no early warning signs. The best way to protect yourself is to have a comprehensive dilated eye exam at least once a year or as directed by your OCB eye doctor. In a comprehensive eye exam, your OCB eye doctor can detect this condition in its earliest changes before it effects your vision. Early intervention can protect you from vision loss.

Who is at Risk?
If you have diabetes you are at risk for diabetic retinopathy. Diabetes comes in two main forms: type 1 and type 2.
In type 1 diabetes, the pancreas is unable to produce insulin, the hormone that enables sugar and other nutrients to leave the bloodstream and enter cells for energy and growth. In Type 2 diabetes, the cells of the body become resistant to insulin and its effects. Both disorders lead to high levels of sugar in the blood, or hyperglycemia. If left untreated, this leads to serious long-term consequences throughout the body, including the eyes.
This chance for developing this eye condition increases as diabetes progresses over time. According to the American Academy of Ophthalmology, after 15 years, 80 percent of people with Type 1 diabetes will develop diabetic retinopathy. After 19 years, up to 84 percent of people with Type 2 diabetes will develop the disease.
If you have diabetes, there are several risk other risk factors, some of which can be managed, that influence the development and severity of diabetic retinopathy including:
Symptoms & Diagnosis
You can have diabetic retinopathy and not be aware of it, since the early stages of the disease don’t cause noticeable symptoms. That is why it is so important to have comprehensive dilated eye exams annually if you have diabetes.
In a dilated comprehensive eye exam, your OCB eye doctor can detect the earliest changes that occur with diabetic retinopathy including:
- Leaking blood vessels
- Retinal swelling (macular edema)
- Fatty deposits in the retina
- Damaged nerve tissue
- Microaneurysms (small, balloon like abnormalities)
As the disease progresses, you may notice any of the following diabetic retinopathy symptoms:
- Spots, dots or cobweb-like dark strings floating in your vision
- Blurred vision
- Vision changes periodically from blurry to clear
- Blank or dark areas in your field of vision
- Poor night vision
- Colors appear washed out or different
- Vision loss
Diabetic retinopathy usually affects both eyes. Contact your OCB eye doctor right away if you experience sudden vision changes or your vision becomes blurry, spotty or hazy.
Treatment
Our fellowship trained OCB retina specialists offer our patients with diabetic retinopathy the most comprehensive and advanced care in laser, medical and surgical options. These treatments don’t cure diabetic retinopathy, but they may slow or prevent progression of vision loss. Without treatment, diabetic retinopathy progresses steadily from minimal to severe stages.
Our team is committed to ensuring that our diabetic patients experience the highest quality of life for many years to come. We want our patients to understand that in its earliest stages, the best treatment for diabetic retinopathy is to manage your diabetes. Be sure you are controlling diabetes in the following ways:
- Strict control of your blood sugar will significantly reduce the long-term risk of vision loss.
- Keep blood pressure and cholesterol levels within normal ranges.
- Smoking increases your risk for developing diabetic retinopathy so if you smoke, quit.
- Eat a healthy, low glycemic diet and exercise regularly. Weight loss is a primary therapy for treating and preventing type 2 diabetes.












